Abstract
Background: Deep vein thrombosis (DVT) is a common diagnosis with a worldwide incidence of 10 million cases per year. The diagnosis requires treatment with anticoagulation that can have both high cost and high risk for bleeding and has traditionally been managed with an inpatient admission. Recent guideline updates from the American Society of Hematology have demonstrated that patients meeting certain criteria can be managed as an outpatient. A retrospective chart review of patients presenting for acute DVT in 2019 demonstrated 58.1% of patients who met criteria for outpatient management were admitted. In order to improve value of care for UF Health patients presenting to the Emergency Department (ED) for acute DVT, a multidisciplinary team consisting of physicians from the departments of Hematology and Emergency Medicine developed a step-by-step ED treatment pathway for the management of acute DVT based on evidenced-based guidelines. The project goal was to achieve less than a 25% admission rate for patient's meeting outpatient management criteria within 1 year.
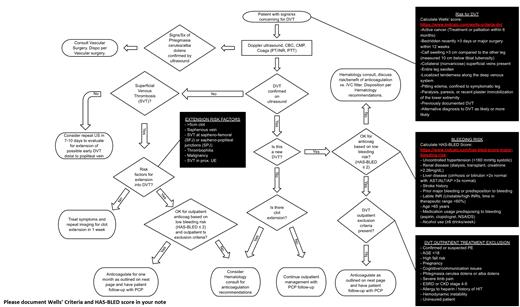
Methods: Recent American Society of Hematology anticoagulation management guidelines supporting outpatient management of DVT presented an opportunity to reduce cost to patients while maintaining safety and improving resource utilization and evidence-based practice. To identify patients that are safe for outpatient management, the HAS-BLED risk stratification tool was implemented. To improve both quality of outpatient treatment and patient compliance, recommended treatment options were updated to reflect current practice standards with an appropriate emphasis on direct oral anticoagulants (DOACs). Finally, a standard documentation template was created for patients being discharged to reduce variation in post-discharge recommendations. A cause-and-effect diagram and interviews were utilized to determine the reasons for patient management decisions including disposition and choice of anticoagulation. These quality improvement tools were added to the ED treatment pathway, which was published in the standard location for similar clinical tools for ED clinicians at our institution. Furthermore, lectures were given at the Emergency Medicine residency conference to educate clinicians on the updates and answer questions.
We subsequently reviewed charts of applicable ED encounters. A run chart was utilized to monitor admission and discharge rates over time. ED encounters with assigned ICD codes for acute and acute-on-chronic lower extremity DVT were reviewed for data collection.
Outcomes: Chart review of ED patient encounters for acute DVT in 2019 demonstrated 255 cases. Of those, 93 patients were identified as meeting criteria for outpatient management. Only 41.9% (n=39) of patients who met criteria for outpatient management were discharged. Unexpectedly, 92% of all encounters did not document bleeding risk. Review of data from January through October 2020 demonstrated an overall decreased incidence of encounters for acute DVT. This is likely a reflection of decreased ED encounters in the setting of the COVID-19 pandemic. Over a 10-month period, 38 patients met criteria for outpatient management. Of these, 76.3% (n=29) of patients meeting criteria for outpatient management for DVT were discharged and 23.7% (N=9) were admitted. This demonstrates a significant improvement in admission rates (59.2% relative reduction) compared to a 58.1% admission rate in 2019 and met our goal of less than 25% admission rate. Furthermore, 89.7% (N=26) of patients who were discharged were prescribed direct oral anticoagulants. Similar to 2019, bleeding risk was documented in only 6.9% of discharged patients. This was an unexpected finding and while not the primary objective of the project, certainly demonstrates a significant opportunity for further care improvements.
Conclusions: The next PDSA cycle will focus on appropriate use of bleeding risk stratification tools and documentation of bleeding risk. Of note, 37.3% of admitted patients who did not meet outpatient management criteria were not discharged because of a concomitant pulmonary embolism. This may present an additional future opportunity for improving value of care for patients with different types of venous thromboembolism.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal